Treating the Tennis Elbow

Lateral epicondylitis, lateral epicondylopathy, lateral epicondylalgia—often known as tennis elbow—affects more than just tennis players. While managing it can be challenging, we will explore key aspects of its diagnosis and treatment
Introduction
Lateral epicondylalgia (LE), commonly referred to as tennis elbow, is a painful condition affecting the tendons of the forearm. While often associated with inflammation, current understanding suggests degenerative processes are at play, making "tendinopathy" a more accurate term than "tendinitis" to describe the condition.
LE has been described as "an overuse injury that occurs secondary to an eccentric overload of the common extensor tendon at the origin of the extensor carpi radialis brevis tendon", as cited by the National Library of Medicine.
This means that in LE, pain is located at the origin of the extensor carpi radialis brevis tendon, which would be pretty hard to locate, so pinpointing the location of pain at the common forearm extensor origin is the way to go. Which lies at the lateral epicondyle of the humerus (hence the name lateral epicondylitis, as it describes pathology at that exact place, which is quite easy to accurately palpate).
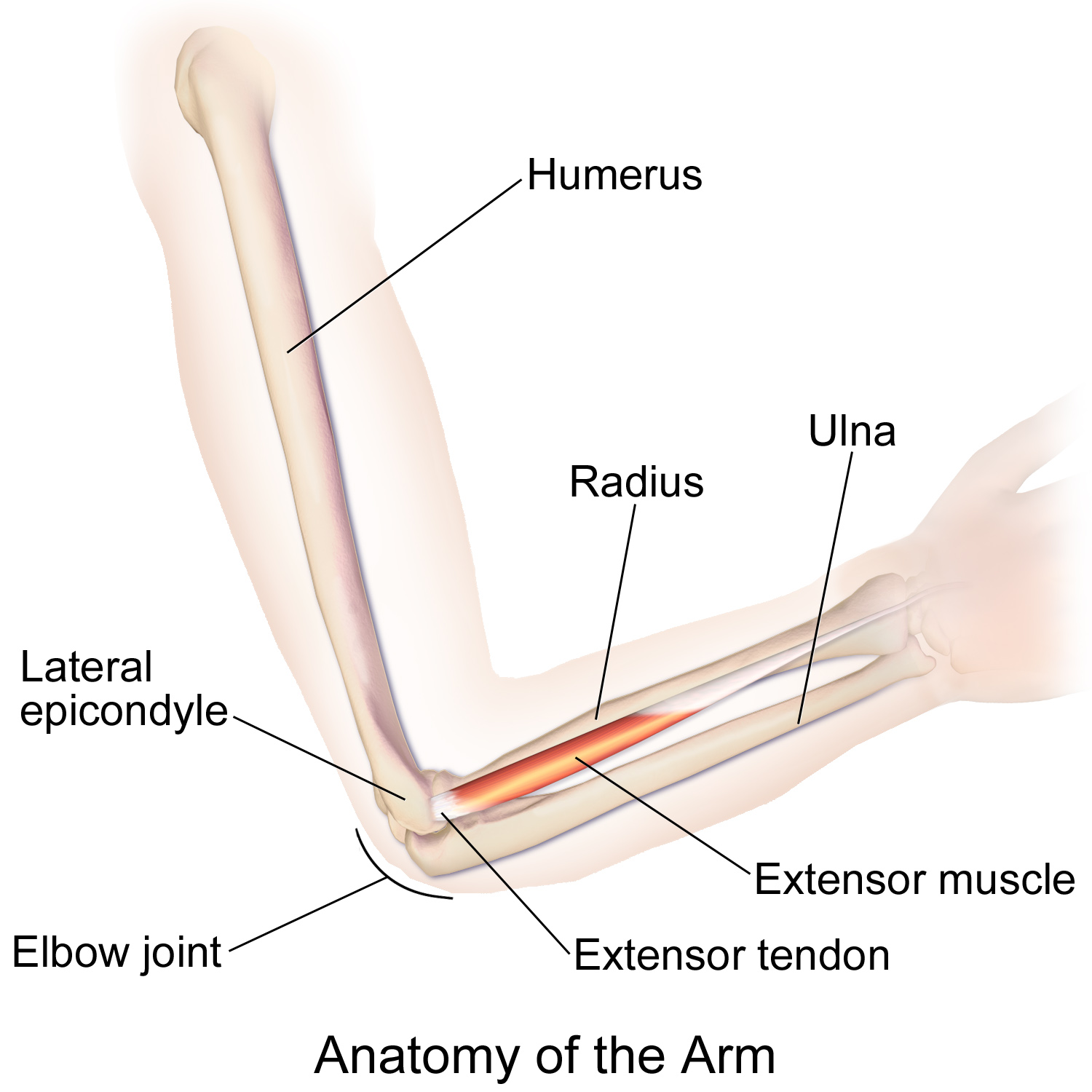
LE is classified as an "overuse injury", often occurring due to repetitive wrist extensions, forearm supinations, or gripping activities that strain the extensor muscles, leading to tendon microtears. These actions, particularly eccentric loading during movements like a tennis backhand (mostly one-handed), can accumulate over time, causing degeneration rather than inflammation.
The same is often true for other sports such as badminton, playing an instrument or performing manual labor.

Although tennis elbow is the name given to the condition, tennis players actually make up a minority (around 10%) of the people affected by the condition nowadays. This is likely due to the rise of the double-handed backhand, which has dramatically reduced the prevalence of LE in the tennis population. The highest chances of seeing someone with LE is usually people between 45 and 55 years, and with a total prevalence of 1.3 percent of the population.
In general, men and women are equally affected by the condition. And with a natural recovery happening in the majority of patients (around 90% of them) over the course of a year, no matter which treatment they underwent.
Main takeaway: LE is a painful condition of the lateral elbow, present in both genders and with incurrence rates in both the athletic and sedentary population.
Pathogenesis:
Now we understand that overuse and not inflammation, drives LE. But how does this degeneration begin?
LE has been described as a degenerative condition (see above). Degeneration refers to the loss of cellular function within tissue, often caused by cumulative microtears in the tendon, due to overuse. These microtears can accumulate if the overload keeps going on for long enough and lead to the tissues degeneration.
When the tendon is stressed beyond its capacity, microtears develop and, over time, lead to functional loss in the tendon. LE can also develop in sedentary individuals who suddenly increase activity, as their underused tendons are less able to handle the stress.
Just as a very high training volume can be problematic for high level athletes in the long run, "normal" exercise can be hard on the sedentary folks.
So, in general, symptoms cannot be associated to a particular traumatic event, but accumulate slowly over time.
Main takeaway: LE develops gradually due to cumulative overload, leading to tendon degeneration. Since the degeneration occurs over time, recovery will also require a gradual process through rehabilitation.
Pathophysiology
The three-component model, proposed by Coombes et al. 2008, that makes up LE:
- Local tendon pathology
- Changes in the pain system
- Impairment in the motor system
This model explains why some cases become chronic, as the condition involves not only structural changes in the tendon but also heightened pain sensitivity due to central sensitization.
This might also explain the high pain level variability between individuals. LE has often been described to show signs of hyperalgesia, which would be in match with changes in the pain system (due to the release of neuropeptides), which can exacerbate the pain response in patients with LE.
Local tendon pathology, as in other tendinopathies, is characterised by neovascularisation, disorganised collagen and increased concentration of neurochemicals. This might be the result of either tendon overuse or underuse, which have both been shown to lead to tendon degradation.
Impairments in the motor systems would include impaired force precision control, which indicates that including fine force control exercises might we a worthy time effort.
All 3 factors are likely present in the more severe LE cases, but to different degrees. Determining which factor is most likely to cause dysfunction in which patient is crucial for successful rehabilitation.
Main takeaway: LE involves three components: local tendon pathology, changes in the pain system (e.g., central sensitization), and motor system impairments. These factors explain why some cases become chronic, with varying levels of severity between patients.

History and Physical Examination:
Patients with LE often include athletes and individuals engaged in repetitive manual labor or musical activities. A thorough history, including occupational factors, is essential for diagnosis.
The clinical history and examination are usually sufficient to make the diagnosis.
To confirm LE, ensure the following clinical features are present:
- Pain is concentrated at the proximal tendon insertion around the lateral epicondyle, with pain often radiating down the forearm.
- Contraction of the extensor muscles reproduces their pain.
- There is a history of overusing the wrist extension (either from sports, manual labor or playing an instrument)
- The wrist musculature gets stressed repetitively
To make the diagnosis, we need to bear in mind what common other causes of lateral elbow pain exist. Most of them have been named in a review paper you can find here.
Differential diagnosis:
Common causes for lateral elbow pain include:
- Lateral epicondylitis (epicondylalgia) = most likely
- Referred pain (from cervical spine, upper thoracic spine, myofascial pain) with pain presenting in elbow and forearm
Less common causes:
- Synovitis of the radiohumeral joint
- Radiohumeral bursitis
- Posterior interosseus nerve entrapment (radial tunnel syndrome). In this case, pain may not be reproduced with wrist extension tests. While resisted supination should reproduce pain due to the supinator muscle being one of the possible areas of nerve compression.
- Elbow overuse due to pathology in an adjacent joint (e.g. frozen shoulder)
Not to be missed: (uncommon)
- Osteochondritis dissecans (in adolescents) of the capitellum radii
People that present with concomitant shoulder or neck pain have poor outcome prognosis.
Experts suggest starting the physical examination at the neck and moving downward, checking each joint for dysfunction. That means the assessment should start at the neck, move towards the shoulders, then the elbow and end at the wrist.
But as easy as it would be, just because someone presents with neck pain and LE, doesn't mean that the LE is coming from the cervical. As it could also be the other way around, that elbow problems led to compensation patterns upstream and that overuse of the spine led to muscular tension or else around the cervical spine.
To rule in LE, make sure that:
- Pain does not spread pain into the hand, fingers or upper arm.
- Pain is related to physical activity, and might have a mechanical origin.
- Pain should be reproduced by resisted elbow extensions.
- Check the cervical spine and upper thoracic region to exclude referred pain as a diagnosis.
(and use the following) Diagnostic tests:
- Mill's Test: = passive palmarflexion and pronation
If the pain can be reproduced, it is likely LE we are dealing with. The test has high reliability and accuracy in diagnosing LE. This test has a specificity of 100%, but low sensitivity. - Maudsley's Test: = middle-finger extension
with a sensitivity score of 88%. - Cozen's Test: = resisted wrist extension
with a sensitivity of 84%, but very low specificity.
To diagnose LE, physical tests like Mill's, Maudsley's, and Cozen's can be used. Mill's test has 100% specificity, ruling out LE if negative. Maudsley's test, involving resisted middle-finger extension, has a sensitivity of 88%, and Cozen's test, with resisted wrist extension, has a sensitivity of 84%.
For a thorough subjective evaluation of a persons pain, use a patient related outcome measure. Precisely the: PRTEE (Patient Related Tennis Elbow Evaluation) which has been shown to be a reliable and valid tool to assess people with lateral epicondylitis.
Imaging techniques:
Most of the time, the diagnosis for LE can be made clinically. In some cases, where after a thorough rehabilitation process no improvements are seen, imaging can be useful.
Radiographs can help exclude bone pathology such as loose bodies, arthritis, or osteochondritis dissecans
Ultrasound is typically the first-line imaging technique for evaluating tendon degeneration.
MRI, though often mismatched with symptoms, can be used to assess other potential causes.
Imaging should be done after undergoing conservative therapy for LE, if the diagnosis can be made clinically. If the diagnosis is uncertain or abnormal, imaging should be encouraged early on. But even then, you need to be careful not to make the findings on the image your diagnosis, if it does not match your physical examination and the clinical presentation of the patient.
Treatment Options
Rest, activity modification, and avoiding painful movements are essential for relieving symptoms of lateral epicondylitis (LE). This includes reducing gripping time and activities that trigger pain, similar to other tendinopathies.
Acute phase treatment: After overloading the extensor muscles, wait before using ice, and only apply it if the pain is unbearable. If tolerable, ice isn't necessary for faster recovery. Consider what activity may have caused the pain and don‘t worry too much about it. In the following days, maintain regular movement but avoid activities that aggravate the pain. After 1-2 weeks of rest, gradually introduce light resistance exercises like hand extensions and flexions.
In general, when symptoms improve after few days, you can start with your normal gym routine but modify your training (e.g. grips) when the stress is too much on the forearm and provokes pain. This does not mean, you should avoid any movements that elicit some pain in the extensors. Pain in the region during normal lifting or normal activities can be 2-3/10.
If you’re a tennis player, or any other athlete, reduce your training frequency, the total time you play each session, or the intensity at which you play. Stay upfront on the court, so you do not get tempted to hit hard. Even when going on the baseline, try to slow down your hitting speed. This can actually be a good time to focus on your technique and play mindfully and not just hitting from the baseline. Place the ball, and don’t just hit it anywhere with speed.
A variety of treatment options have been recommended for LE. Unfortunately, there are still no universally accepted therapeutic modalities (discussed below).
General treatment goals: Treatment for LE aims to control pain, maintain range of motion, improve grip strength and endurance, restore normal function, and prevent further damage.
Nonoperative treatment remains the priority and mainstay for most patients with LE. Surgery can be an option, although is not recommended.
Monitoring exercise: Pay attention to pain during, immediately after, and the day following exercise. Ask yourself:
- Is the pain tolerable during exercise (aim for a 2-3/10 on the pain scale)?
- Does the pain improve, worsen, or stay the same after exercise?
- How is the pain the next day?
For example, you rate your pain on day 1 when squeezing a ball as a 2/10 pain. You then perform your exercise routine within tolerance, go about your day, and go to bed without any major issues. The next morning you squeeze the ball again, but this time you rate your pain as a 5/10. This means that even though your symptoms were tolerable during exercise, you might have done more than what you can currently recover from. You didn’t do any harm, but decreasing the volume or intensity of exercise would be recommended.
What are interventions if pain persists?
Slow progressive resistance training should do the job right?
Maybe!?
Exercise: Isotonic or isometric exercises are missing standardized protocols and therefore clinically relevant studies. They can help in restoring strength without little pain in the short term, but long term outcomes are still missing.
Exercise therefore has similar effects as the other non-invasive treatment options: short term pain relief with a lack of knowledge regarding long term effects on pain, strength , disability and quality of life.
Regardless of dosage, exercise is effective in reducing pain in LE; however, due to lack of comparison between dosing parameters, the optimal dosage is unclear. All exercise variations showed some degree of improvement in pain and function; however, no major differences were found between the types of exercises (Kinney & Anderson, 2023).
Eccentric exercises were traditionally believed to be the best approach for LE, but the systematic review and meta-analysis by Karanasios et al. (2020) showed “no difference between concentric–eccentric and eccentric exercise alone…”. Just perform every exercise slowly and with control. They also concluded that there is still low certainty, if exercise is better in pain outcomes than wait-and-see approach.
Other non-invasive treatment options including manual therapy, taping, bracing, injections, electrophysical modalities, acupuncture or oral NSAID’s are also quit inconclusive and rather contradicting in their long term benefit. (Campos et al., 2024; Stasinopoulos, 2022).
Classic physiotherapy: Landesa-Piñeiro and Leirós-Rodríguez (2022) examined physiotherapy treatments for tennis elbow, including exercise, manual therapy, taping, shockwave therapy, and immobilization, focusing on pain, functionality, and grip strength. For acute tennis elbow (<3 months), all treatments except immobilization improved pain and functionality, while exercise, manual therapy, and shockwave therapy also enhanced grip strength. The authors recommend these therapies for acute cases as they benefit all three outcomes. However, there is limited evidence on their effectiveness for chronic tennis elbow and long-term results. They also noted that the inclusion of non-controlled and non-randomized studies weakened the validity of their conclusions, highlighting the need for further research to establish evidence-based treatments.
Taping: Current evidence suggests that kinesiology taping may help reduce pain and improve elbow joint function in patients with lateral epicondyle tendinopathy in short-term, with potential clinical significance. Physiotherapists can consider using kinesiology taping as a treatment option for patients with lateral epicondylitis (Li et al., 2024). As mentioned above, long term outcomes are missing.
Wait-and-see: Lapner et al. (2022) compared strengthening, corticosteroids (CS), platelet-rich plasma (PRP) and autologous blood (AB) with wait-and-see treatment or placebo control in patients with lateral epicondylitis. It was the only study with long term outcome measure, with the duration of 6-12 months for follow-up. Strengthening, PRP, and AB had the same pain and functional score outcome as the wait-and-see approach. CS revealed worse long-term pain and functional outcomes than the placebo group.
Acupuncture: There does not seem to be a direct answer, whether acupuncture helps or not in treating tennis elbow. As some systemic reviews say yes, others say no (Ma & Wang, 2020). Some studies indicate, short term pain-relieve, others don’t. The conclusion of the meta-analysis by Zhou et al. (2020) was like: the heterogeneity of treatment protocols and to much bias in the methods of clinical trials, make it difficult to establish a consensus whether the treatment is effective or not, further no studies in the meta-analysis included a long term follow up.
Electrophysical modalities: Dingemanse et al. (2013) looked at the effectiveness of electrophysical modalities (ultrasound, extracorporeal shock wave therapy (ESWT), transcutaneous electrical nerve stimulation (TENS), laser therapy). There is inconclusive and/or conflicting evidence for the use of any modality for acute or chronic stages of tennis elbow. A more recent umbrella review by Kinney and Anderson (2023), investigating nonoperative management of lateral epicondyle tendinopathy, also found inconsistent results for passive modalities (shockwave therapy, ultrasound, and laser). Though the systematic review and meta-analysis by Yao et al. (2020) show beneficial effects of shock wave therapy compared to other modalities, other reviews showed no differences to placebo treatments (Cheema et al., 2023; Yao et al., 2020). These different outcomes may be explained by methodological differences among studies, including the number of shock wave pulses delivered, pulse frequency, duration of application, follow-up duration, treatment interval, specific devices used and evaluation methods.
However, the efficacy of shockwave therapy for tennis elbow remains controversial, as some studies have reported that shock wave is highly effective and even a reasonable alternative to surgery, while others have reported effects not markedly different from placebo. That means, mixed results for shock wave therapy. It may come down to believes and luck with the right application form.
Manipulation: What about manipulation, friction massage or soft tissue mobilization? The current evidence speaks for short-term outcome improvements, but midterm and long-term outcomes are still unknown. Given the vide variety of techniques in manipulating the skin, it is unknown which technique is superior over others. There is simply a lack of high-quality RCTs comparing specific manual therapy soft tissue techniques against a true control group while using the same outcome measures. Soft tissue mobilizations can, in combination with exercise, improve outcomes but based on conflicting evidence, a recommendation as a standalone treatment cannot be made (Lucado et al., 2022).
Injections: The systematic review and meta-analysis by Houck et al. (2019) and Tang et al. (2020) questioned the effectivness of autologous blood, platelet-rich plasma or corticosteroid injections for tennis elbow. They concluded that the current best available evidence suggests that CSI improves functional outcomes and pain relief in the short term, while AB and PRP are the most effective treatments in the intermediate term, but there is currently strong evidence that PRP injections are not efficacious for chronic tennis elbow (Kinney & Anderson, 2023).
Even though hyaluronic acid seems pretty promising, there are simply not enough studies to confirm the positive effects and superiority over other injections (Dong et al., 2015; Zinger et al., 2022; Kinney & Anderson, 2023).
Surgery: Tennis elbow symptoms seem to have a half-life of about 3-4 monhts ON AVERAGE, meaning that symptoms were either much better or had resolved completely at every following 3-4 months. On the individual level this can mean quicker elevations of symptoms or longer durations of symptoms. So symptoms could be largely irrelevant and provide little prognostic value, as future course of symptom relieve is completely unpredictable. Recovery seems to be a random process. So the challenge with nonoperative treatment is that we can not predict who will fail or when treatment has truly failed. Moreover, failure of nonoperative methods doesn’t guarantee surgery will be effective. Advising surgery based on time alone is unjustified without strong evidence from randomized controlled trials, which is currently lacking (Karjalainen & Buchbinder, 2023).
About 90% of patients recover within a year without treatment, regardless of how long symptoms have lasted before. Patients with persistent symptoms should know that improvement is just as likely later as it was early on. Duration alone shouldn’t justify surgery, and failed nonoperative treatment shouldn't justify surgery unless we can reliably identify those who won’t recover without it (Ikonen et al., 2021).
General Guideline
When experiencing lateral elbow tendon pain, decrease the amount of pain provoking activity (hard gripping, fast repeated twisting, fast accelerated/decelerated wrist extension/flexion). After 2-3 Weeks, steadily increase the activities again. Do not get frustrated if symptoms stay the same or just decrease slightly, as pain and function improve over time on it’s own without adjunct treatment.
For amateur athletes this should be no problem. Elite Athlete, who eventually do get tendon overload pain, will need to use the same approach, but can add motor imagery training into their rehabilitations program. It does not stress tissue and maybe has performance enhancing effects, but this has to be clarified in the future (Deng et al., 2024).
Evidence is lacking regarding the superiority of one nonoperative treatment option over another, and past systematic reviews and meta-analysis have not reached definitive conclusions. The best approach for this tendon pain is highly individual, but we recommend starting with progressive exercise training with taping, as it is the most cost-effective strategy (bonus effects from exercise). If you decide to do nothing, literature can’t argue with that.
If you want to dive deeper in the literature of later elbow tendon pain, Di Filippo et al. (2022) lists all treatment interventions. Lucado et al. (2022) and Kinney and Anderson (2023) describe the current evidence for all this treatments.
References:
Campos, M. G., Maia, L. B., Mascarenhas, R. O., Lourenço, B. M., Henschke, N., & Oliveira, V. C. (2024). Effectiveness of non-invasive therapies on pain, maximum grip strength, disability, and quality of life for lateral elbow tendinopathy: A systematic review and meta-analysis. Brazilian Journal of Physical Therapy, 28(2), 100596. https://doi.org/10.1016/j.bjpt.2024.100596
Cheema, A. S., Doyon, J., & Lapner, P. (2023). Transcutaneous electrical nerve stimulation (TENS) and extracorporeal shockwave therapy (ESWT) in lateral epicondylitis: a systematic review and meta-analysis. JSES International, 7(2), 351–356. https://doi.org/10.1016/j.jseint.2022.11.002
Deng, N., Soh, K. G., Abdullah, B. B., & Huang, D. (2024). Does motor imagery training Improve service Performance in tennis Players? A Systematic Review and Meta-Analysis. Behavioral Sciences, 14(3), 207. https://doi.org/10.3390/bs14030207
Di Filippo, L., Vincenzi, S., Pennella, D., & Maselli, F. (2022). Treatment, Diagnostic Criteria and Variability of Terminology for Lateral Elbow Pain: Findings from an Overview of Systematic Reviews. Healthcare, 10(6), 1095. https://doi.org/10.3390/healthcare10061095
Dingemanse, R., Randsdorp, M., Koes, B. W., & Huisstede, B. M. A. (2013). Evidence for the effectiveness of electrophysical modalities for treatment of medial and lateral epicondylitis: a systematic review. British Journal of Sports Medicine, 48(12), 957–965. https://doi.org/10.1136/bjsports-2012-091513
Dong, W., Goost, H., Lin, X., Burger, C., Paul, C., Wang, Z., Kong, F., Welle, K., Jiang, Z., & Kabir, K. (2015). Injection therapies for lateral epicondylalgia: a systematic review and Bayesian network meta-analysis. British Journal of Sports Medicine, 50(15), 900–908. https://doi.org/10.1136/bjsports-2014-094387
Houck, D. A., Kraeutler, M. J., Thornton, L. B., McCarty, E. C., & Bravman, J. T. (2019). Treatment of lateral epicondylitis with autologous blood, Platelet-Rich plasma, or corticosteroid injections: A Systematic review of overlapping meta-analyses. Orthopaedic Journal of Sports Medicine, 7(3), 232596711983105. https://doi.org/10.1177/2325967119831052
Ikonen, J., Lähdeoja, T., Ardern, C. L., Buchbinder, R., Reito, A., & Karjalainen, T. (2021). Persistent tennis elbow symptoms have little prognostic value: A systematic review and meta-analysis. Clinical Orthopaedics and Related Research, 480(4), 647–660. https://doi.org/10.1097/corr.0000000000002058
Karanasios, S., Korakakis, V., Whiteley, R., Vasilogeorgis, I., Woodbridge, S., & Gioftsos, G. (2020). Exercise interventions in lateral elbow tendinopathy have better outcomes than passive interventions, but the effects are small: a systematic review and meta-analysis of 2123 subjects in 30 trials. British Journal of Sports Medicine, 55(9), 477–485. https://doi.org/10.1136/bjsports-2020-102525
Karjalainen, T., & Buchbinder, R. (2023). Is it time to reconsider the indications for surgery in patients with tennis elbow? The Bone & Joint Journal, 105-B(2), 109–111. https://doi.org/10.1302/0301-620x.105b2.bjj-2022-0883.r1
Kinney, W. R., & Anderson, B. R. (2023). Nonoperative Management of Lateral Epicondyle Tendinopathy: An umbrella review. Journal of Chiropractic Medicine, 22(3), 204–211. https://doi.org/10.1016/j.jcm.2023.04.004
Landesa-Piñeiro, L., & Leirós-Rodríguez, R. (2022). Physiotherapy treatment of lateral epicondylitis: A systematic review. Journal of Back and Musculoskeletal Rehabilitation, 35(3), 463–477. https://doi.org/10.3233/bmr-210053
Lapner, P., Alfonso, A., Hebert-Davies, J., Pollock, J. W., Marsh, J., & King, G. J. W. (2022). Nonoperative treatment of lateral epicondylitis: a systematic review and meta-analysis. JSES International, 6(2), 321–330. https://doi.org/10.1016/j.jseint.2021.11.010
Li, Y., Mei, L., Rahat, S., Pang, L., Li, R., Xiong, Y., Li, J., & Tang, X. (2024). The efficacy of kinesio tape in patients with lateral elbow tendinopathy: A systematic review and meta-analysis of prospective randomized controlled trials. Heliyon, 10(3), e25606. https://doi.org/10.1016/j.heliyon.2024.e25606
Lucado, A. M., Day, J. M., Vincent, J. I., MacDermid, J. C., Fedorczyk, J., Grewal, R., & Martin, R. L. (2022). Lateral elbow pain and muscle function impairments. Journal of Orthopaedic and Sports Physical Therapy, 52(12), CPG1–CPG111. https://doi.org/10.2519/jospt.2022.0302
Ma, K., & Wang, H. (2020). Management of Lateral Epicondylitis: A Narrative Literature review. Pain Research and Management, 2020, 1–9. https://doi.org/10.1155/2020/6965381
Stasinopoulos, D. (2022). Isometric exercise for the management of lateral elbow tendinopathy. Journal of Clinical Medicine, 12(1), 94. https://doi.org/10.3390/jcm12010094
Tang, S., Wang, X., Wu, P., Wu, P., Yang, J., Du, Z., Liu, S., & Wei, F. (2020). Platelet‐Rich plasma vs Autologous blood vs corticosteroid injections in the treatment of lateral epicondylitis: A Systematic Review, Pairwise and Network Meta‐Analysis of Randomized Controlled Trials. PM&R, 12(4), 397–409. https://doi.org/10.1002/pmrj.12287
Yao, G., Chen, J., Duan, Y., & Chen, X. (2020). Efficacy of Extracorporeal shock wave therapy for Lateral Epicondylitis: A Systematic Review and Meta-Analysis. BioMed Research International, 2020, 1–8. https://doi.org/10.1155/2020/2064781
Zhou, Y., Guo, Y., Zhou, R., Wu, P., Liang, F., & Yang, Z. (2020). Effectiveness of Acupuncture for Lateral Epicondylitis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Research and Management, 2020, 1–10. https://doi.org/10.1155/2020/8506591
Zinger, G., Bregman, A., Safran, O., Beyth, S., & Peyser, A. (2022). Hyaluronic acid injections for chronic tennis elbow. BMC Sports Science Medicine and Rehabilitation, 14(1). https://doi.org/10.1186/s13102-022-00399-0