Patellar tendinopathy - Treatment protocol

Patellar tendinopathy (PT), or more commonly 'jumper's knee', can be a debilitating injury in lower-body dominant sports such as basketball and volleyball. Here we discuss how to manage this injury.
The quadriceps consists of 4 different muscles – the vastus medialis, vastus lateralis, vastus intermedius, and rectus femoris. All four muscles come together to form the quadriceps tendon that attaches to the patella, or kneecap. They’ll then insert on the tibial tuberosity via the patellar tendon and act to extend or straighten the knee. Together, they’re referred to as the knee extensor mechanism. Therefore, any time your quads are working, such as when squatting, jumping, running, and climbing stairs, your patellar tendon is also working.
Patellar tendinopathy is a source of anterior knee pain, characterised by pain localised to the inferior pole of the patella. Pain is aggravated by loading and increased with the demand on the knee extensor musculature, notably in activities that store and release energy in the patellar tendon (Aicale et al., 2020). Repetition of this spring-like activity over a single exercise session, or with insufficient rest to restore the tendon helath between sessions, can induce pathology and a change in the tendon’s mechanical properties, which is a risk factor for developing symptoms (Malliaras et al., 2015). As with the Wolff’s law and bone remodelling, the same mechanism works for soft tissues (Davis’s law). Structures adapt to imposed demands.
Inflammation of the tendon could occur when there is overuse during athletic activities, although this can be return to normal when the load is adjusted. However, when high load persists, the injury can become chronic (Theodorou et al., 2023). This could mean increases in tenocyt numbers, causing matrix degeneration, neovascular ingrowth and swelling (all symptoms and factors for tendon pathology) (Malliaras et al., 2015). The exact mechanism of tendinopathy and the theories behind the phenomenon will be discussed in another article
Prevalence
The overall prevalence of PT in elite players from nine different sports is 14.2% and in non-elite sports the overall prevalence was 8.5%.
For the non-elite level, the highest prevalence was in volleyball players (14.4%) and basketball (11,8%). In the elite-level, the same can be said, as volleyball with 45% and basketball with 32% have the highest prevalence in different sports (Theodorou et al., 2023).
The prevalence of men with PT (25.3%) was significantly higher in comparison to women (13.1%). This can be explained by the fact that women’s patellar tendons are exposed to lower forces because they have less quadricep strength and an inferior jumping capacity (Theodorou et al., 2023).
Also, PT epidemiology varied by age, with a prevalence of 10.1% in younger athletes and doubling to 21.3% in older athletes. Interestingly enough is the fact that the general population only indicates a prevalence and incidence for PT of only 0.1% (Nutarelli et al., 2023). Therefore the participation in sports is a risk factor for PT and it could be assumed that the number of training hours is an additional risk factor for developing PT.
Risk factors
Van der Worp et al. (2011) looked for risk factors associated with PT and found no good evidence for any factor. The only moderate evidence comes from body weight and BMI. The apparent association of weight and BMI with PT can be explained by a higher body mass theoretically leading to a higher loading of the patellar tendon, which increases changes of overload.
While certain intrinsic risk factors for patellar tendinopathy have been identified, such as gender, weight and body mass index, the most significant risk factor appears to be training load (i.e. an extrinsic risk factor).
Biomechanical factors, contributiong to overload in the tendon are discussed in the following section "contributing factors".
Diagnosis
The diagnosis of patellar tendinopathy is clinical. Differential diagnoses for patellar tendinopathy would include other causes of anterior knee pain such as quadriceps tendinopathy, patellofemoral pain syndrome, Hoffa’s fat pad pathology, meniscal injury, bursitis, osteochondral injury, Osgood-Schlatter disease and Sindig-Larsen-Johansson syndrome.
The first clinical challenge is to establish whether the tendon is the source of the patient’s symptoms. As mentioned above, patellar tendinopathy is one of many potential diagnoses producing anterior knee pain and it has specific features that consist of (1) pain localized to the inferior pole of the patella and (2) load-related pain that increases with the demand on the knee extensors, notably in activities that store and release energy in the patellar tendon. Other signs and symptoms, such as pain with prolonged sitting, squatting, and stairs, may be present but are also features of patellofemoral pain (PFP) and potentially other pathologies. Tendon pain occurs instantly with loading and usually ceases almost immediately when the load is removed. Pain is rarely experienced in a resting state. Pain may improve with repeated loading (the “warm-up” phenomenon), but there is often increased pain the day after energy storage activities. The dose-dependent pain is a key feature, and assessment should demonstrate that the pain increases as the magnitude or rate of application of the load on the tendon increases. The paper from Silva et al. (2023) developed clinical guidelines to incrementally increase the rate and magnitude of patellar tendon loading. If pain increases with patellar tendon loading, the chance for patellar tendinopathy seems strong. The single leg decline squat test has proven it’s usefulness in practise to evaluate patellar tendinopathy as it elicits the greatest tendon load. This test is performed by having the patient stand on a board tilted at 25° and squat on the affected leg until pain is felt (usually already at 30° flexion).
Next to pain location and pain severity at different load variations, the VISA-P questionnaire is a tool used to assess the severity of symptoms as well as to monitor outcomes. The VISA-P is a 100-point scale, with higher scores representing better function and less pain. The minimum clinically important difference is a change of 13 points (Malliaras et al., 2015).
The VISA-P-G is a reliable and valid questionnaire for the self-assessment of pain, symptoms, and function in German-speaking patients with patellar tendinopathy (Lohrer & Nauck, 2011).
However, a recent systematic review by Korakakis et al. (2021) of the VISA questionnaires showed very-low-quality evidence for their validity. Furthermore, a recent reliability meta-analysis from Palazón-Bru et al. (2020) claims that greater evaluation with more scientific evidence is required before it can be implemented in clinical practice.
So, on one hand the questionnaire seems to be validated but on the other hand it’s not.
Patellar tendon imaging does not confirm patellar tendon pain, as pathology observed via ultrasound imaging may be present in asymptomatic individuals (Malliaras & Cook, 2006; Malliaras et al., 2006).
Therefore, repeated imaging is not recommended, as symptoms often improve without corresponding changes in pathology on ultrasound imaging or magnetic resonance imaging. However, imaging can be helpful to include or exclude potential alternate diagnoses of anterior knee pain when the clinical picture is unclear (Malliaras et al., 2015). Remember, imaging can tell us about structure and pathology but not about pain. You can not image pain.
What about palpation?
Cook et al. (2001) evaluated the validity of tendon palpation in the diagnosis of the condition and reported a sensitivity of 68% and low specificity of 9% when comparing to visible lesions on Ultrasound. Maffulli et al. (2017) evaluated the same test (Royal London Hospital Test) and found a sensitivity of 98% and a specificity of 94%. However, the clinical value as a standalone test remains moderate.
To conduct the test, the patient lies in supine and the patella tendon is palpated for local tenderness from proximal to distal while the knee is extended. Once local tenderness is felt, the tender portion of the tendon is again palpated but now with the knee bent to 90°, which places the tendon under tension. The test is considered positive if the pain is markedly reduced or absent in knee flexion. The reason why symptoms decrease with the tendon under tension is unknown. Pain during palpation may not indicate clinical tendinopathy as asymptomatic tendons can test positive during palpation (Cook et al., 2001). Further, the patellar tendon has been shown to be a highly sensitive area to pressure in patients with knee osteoarthritis suggesting that palpation may not be specific to patellar tendinopathy (Van Ginckel et al., 2016; Hannington et al., 2020). Furthermore it is also important- as for every palpation diagnosis – the experience of the therapist to palpate "correctly“.
Differential Diagnosis
As mentioned before, patellar tendinopathy does not seem to be the solely driver of anterior knee pain and needs some further evaluation.
The age of the patient is also important to assist in making the diagnosis. In skeletally immature individuals, abnormal loading of the patellar tendon caused by chronic repetitive stress leads to Sindig-Larsen-Johansson syndrome, which is a traction apophysis injury at the inferior pole of the patella or Osgood-Schlatter disease, a traction apophysis at the tibial tuberosity (Drakes, 2023). Traction apophyses are bony outgrowths that form at the sites where tendons attach to bones. These outgrowths develop due to repetitive pulling forces during childhood growth when bones are still developing (Corbi et al., 2022).
Example of differential diagnosis: patellar tendinopathy vs. quadriceps tendinopathy
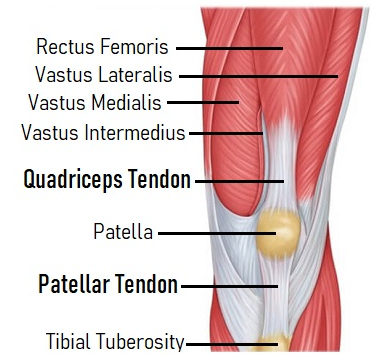
Jumper’s knee is not synonymous with patellar tendinopathy. The term includes patellar tendinopathy and quadriceps tendinopathy. Although the patellar and quadriceps tendons work together as part of the extensor mechanism of the knee, they have distinct anatomical and functional roles. The patellar tendon attaches bone to bone, whereas the quadriceps tendon attaches muscle to bone. The patellar tendon connects 2 structures of similar stiffness, whereas the quadriceps tendon connects 2 structures with different stiffness. Tendon has greater flexibility / extensibility (less stiffness) at the region closest to the muscle. Conversely, regions closer to the bone are less extensible (stiffer). Due to the difference in attachment sites, the patellar tendon is stiffer than the quadriceps tendon. There are differences in structure between the patellar tendon and quadriceps tendon. The patellar tendon is a relatively linear structure, composed of superficial and deep layers, running in parallel without direct muscular attachments. The superficial layer is the extension of the quadriceps tendon fibers from the rectus femoris. Fibers of the deep layer begin at the most distal aspect of the patella and insert, along with the superficial fibers, at the tibial tuberosity. In contrast, the quadriceps tendon is a more complex and variable structure, arising from 4 separate muscles. Typically, the quadriceps tendon has 3 layers: a superficial layer (rectus femoris), intermediate layer (vastus lateralis and medialis), and deep layer (vastus intermedius). Each quadriceps muscle has a unique line of action, subjecting the quadriceps tendon to nonuniform load. The force transmitted through the patellar tendon is more uniform.
Patellar tendinopathy presents as pain at the inferior pole of the patella. Conversely, quadriceps tendinopathy presents as pain at the superior pole of the patella, with symptoms most pronounced with deep knee flexion. The initial onset of symptoms is usually related to an acute incident involving high levels of eccentric quadriceps loading, which occurs, for example, with knee flexion when landing from a rebound in basketball. However, symptoms are typically preceded by a period of excessive load. Although few studies have examined the prevalence of quadriceps tendinopathy, the prevalence estimates range from 0.2% to 2% in athletic populations (Sprague et al., 2019).
All tendinopathies, including patellar and quadriceps tendinopathies, are overuse injuries resulting from tendon overload with inadequate recovery, but treatment could be different as the patellar tendon and quadriceps tendon are not loaded equally throughout knee motion. The quadriceps tendon experiences greater loads than the patellar tendon when the knee moves further into flexion. This relationship is due to an increasing mechanical advantage of the patellar tendon and greater passive tension in the quadriceps muscle as it approaches end range. This may explain why pain in quadriceps tendinopathy is most felt in activities that involve deep knee flexion. Loading programs for quadriceps tendinopathy should include appropriate loading in deep knee flexion. However, due to the lack of literature on quadriceps tendinopathy, there are no specific treatment options available (Sprague et al., 2019).
Exercise rehab
Patellar tendinopathy involves pain that worsens with increased load on the knee extensors, especially during activities that strain the patellar tendon (Malliaras et al., 2015).
This tells us two things:
Patellar tendinopathy pain occurs with loading and subsides once the load is removed. This also means that stopping the pain-provoking exercise would be the easiest way to keep a person pain-free.
Secondly, pain is load-dependent. Which means that the more load you expose your patellar tendon to, the more painful it will get.
So, why would we want to exercise an already injured tendon?
Tendons, like muscles, adapt to the load they are subjected to. Which means, that if we stop loading a tendon completely (like getting into a wheelchair), our pain will be gone for sure, but our tendon will adapt to the environment of "no stimulus" and therefore break down unnecessary tendon tissue, making the structure even weaker than it already is. So that the next time you stand up, pain will be triggered by even less load, as your tendons "loading capacity" has been strongly reduced.
Luckily, it also works the other way around. And that premise builds the core principle of tendon rehabilitation. To desensitize the irritated tendon, we reduce the load by avoiding pain-provoking activities. We do that by switching them out with less pain-provoking exercises, that focus on building up quadriceps strength and patellar tendon loading-capacity, which then lets our tendon become stronger and more tolerable for loading over time, without pain triggering that fast. Since tissues take time to adapt, this exercise approach, which has the highest level of evidence for treating tendinopathies, will take several months for full symptom resolution.
Clearly explaining the rehabilitation process and setting realistic expectations with patients is crucial. Inform them that tendinopathy recovery is a gradual process, typically requiring several months, and there are no quick fixes.
Contributing factors:
It is recommended to perform a complete physical examination of the lower-extremity, to look out for possible contributing factors that we might want to clear, next to our training protocol.
We want to look out for flexibility deficits in the hamstrings or quadriceps muscles and perform stretches if muscles are tight, as they have been shown to contribute to the condition (Dimitrios et al., 2012). As well as dorsiflexion ROM, because a decrease in dorsiflexion will reduce the ankles shock absorption, putting more strain towards the knee.
Jumping technique: Make sure that your patients (if they perform sports where jumping is relevant) don't land too stiffly (Malliaras et al., 2015). We want them to have a smooth landing, that involved ankle dorsiflexion, knee flexion and hip flexion all to a visible degree. As the force put onto the patellar tendon during landing is affected by the position of the trunk.
We can cue this with: "land as silently as you can" or "lean your upper body forward", which will hopefully improve load distribution among the three primary lower limb joints.
Strength testing for the quadriceps, hamstrings, glutes and gastrocnemius either via hand-held dynamometry or by performing exercises for max repetitions single-legged and then comparing side-to-side results (e.g. single-leg heel raises for the calf).
Loading modification:
A patient presenting with patellar tendinopathy will very likely be in pain due to either a lack of variation in an exercise program (over-specificity) which involves repeatedly applying the same stresses too often. Or over the long term, if loading, volume, or intensity increases beyond what tendons can handle, it results in overuse. On the other hand, sudden changes in exercise programming that introduce new and unaccustomed loads can also cause short-term overload.
Therefore, to make workouts more tolerable we can try varying an athletes exercise regime. If a particular exercise worsens your tendinopathy, consider switching to a different movement temporarily until the symptoms improve.
This often requires us to get rid of high-energy storing exercises, that trigger a pain-reaction. While reducing overall volume, training frequency and intensity, if necessary, for desensitisation to take place. But as we will see below, not all plyometric exercises will be more straining for the patellar tendon than different squatting variations.
But to be clear, with "loading modification", by all means we don't mean to quit every activity that provokes some pain. You can keep performing any activity that keeps your pain below a 4 out of 10 pain scale (pain is generally accepted but should not be breath taking), so when the pain starts to increase to a point where you start to make a grimace, it's too much.
We just need to get rid of the most pain-provoking exercises, reducing overall volume to create a recovery environment for the tendon, while loading it with appropriate exercises that will facilitate the healing response. Authors suggest that pain is acceptable, as long as symptoms resolve back to baseline over the next 24-hours (Malliaras et al., 2015). If that is not the case, intensity needs to be further reduced.
When things start to hurt and we try to help by adding therapeutic exercises, the problem can get worse. Which is why we will need to focus on changing exercises while reducing overall training volume. This can be done by applying different training approaches, that might be new to the patient or athlete. But we need to be thinking about our patients complete training program if we want to make a difference.
To maintain cardiovascular and pulmonary fitness, engaging in cross-training activities that place less stress on the tendons is appropriate. For athletes in jumping sports like volleyball and basketball, this could mean opting for activities such as cycling, swimming, or pool running instead of overground running and jumping (Reinking, 2016).
Rehab Stages:
After understanding the importance of loading modification, let's explore the specific stages of rehabilitation.
Rehabilitation of patellar tendinopathy is often split up into 4 stages:
- Isometric exercises
- Isotonic exercises
- Energy-storage exercises
- Progressive return to sport
While this approach might be useful for high-level athletes with a highly provocative tendon, it is not the way to go about tendinopathy for recreational weightlifters, our weekend-warriors or other less "sports-oriented" populations.
In order to adapt these 4-stages for a broader population, we suggest the following stages be adapted:
- Loading modification
- Isotonic exercises
- Lifestyle changes
- Progressive return to sport
This stems from 2 assumptions:
- Isometric exercises are not that important for the rehabilitation of tendons as we think they are, but more about that below.
- Painful conditions always warrant us to not only look at the tissues from a biomedical perspective, but to take a bio-psycho-social view-point.
These changes in the treatment approach in an update on what we currently know about tendons and painful conditions in general, and gets us to look at more than just the training aspect when a patients presents themselves to us.
Stage 1 includes: Both low level exercises with the overall volume reduction (loading modification), while managing some of the physically asses restrictions, if present, such as strength or flexibility deficits of the surrounding musculature and working on technique improvements (e.g. jumping quality).
It's crucial to avoid completely stopping activities, as this can further reduce the tendon's loading capacity.
Stage 2: For the more painful tendons, restricting knee ROM for the initial ranges of flexion is ideal at first.
On the training days, Heavy slow resistance (HSR) training is recommended. While training should not be too pain provoking, it still needs to be challenging enough to elicit a training response (adaptation). We recommend performing HSR in the 6-15 rep range, starting out on the higher end and then lowering repetitions and increasing weight over time. Repetitions should focus on slow repetitions (as the name suggests), where the weight is controlled (e.g. 3-0-2 rhythm).
These exercises should be performed even after "return to sport" for at least 2 times per week for 1 year.
Stage 3: Lifestyle factors, such as sleep, eating habits, mental well-being, social environment and so on need to be assessed to aid recovery. This stage emphasises realising that a person is not a tendon (duh). And a variety of factors can lead to either increased or reduced performance or pain levels.
Stage 4: Once good strength and therefore a good load tolerance has been achieved, return to sports can be initiated (following return to full training without symptom provocation). Except for the people, where simply reducing the training frequency and load (as in weightlifting) was enough to calm down the symptoms in the first place, then the sport has never been quit in the first place (maybe a change in exercises and technique).
For the rest, old exercises can slowly be built up with maybe more "intelligent" monitoring of exercise progression and implementation of taper phases.
To illustrate return to sports: a jumping athlete might begin with 3 sets of 8 to 10 low-intensity jumps and landings, where the jumps are not very high and the landings are shallow. As the athlete becomes more tolerant, the number and difficulty of both the low-intensity jumps and split squat jumps can be progressively increased based on individual goals. Ultimately, higher-intensity exercises can be introduced to match the volume and intensity of sport-specific training. These exercises could include single-leg hops, forward hops, deeper split squat jumps, and sport-specific jumps like those used for blocking and spiking in volleyball.
In summary:
| Stage | Description |
|---|---|
| Loading Modification | Reduce load and avoid high-stress activities |
| Isotonic Exercises | Controlled, slow resistance exercises |
| Lifestyle Changes | Sleep, diet, stress management |
| Progressive Return to Sport | Gradually reintroduce sports-specific activities |
Are isometrics really necessary?
Isometrics and tendon pain. They have recently been presented to be one hell of a couple we all need to include into therapy. But why so?
Isometrics have shown to be highly analgesic (=leading to a reduction in pain) for the patellar tendon in a 2015 study from Rio et al. But these findings couldn't be replicated in later research.
But apart from that, the question remains: do we even want to present our patients an option to be pain free immediately (if it existed)?
This might sound like we don't want to rid our patients of pain, but that's not the case. First of all, there is evidence, that isotonic exercises are as analgesic as isometric exercises in the short and long-term (Van Ark et al., 2016). And secondly, even if isometrics would reduce symptoms more efficiently short-term, then our patients would likely think of the possibility of there being a "quick-fix" for their condition. Even if it has been repeatedly shown to take several months to fully cure any tendinopathy and we want to focus on improving function and tendon architecture, not on temporary pain-relief. And experiencing pain during training is not detrimental for recovery, as Karin Silbernagel and colleagues point out in an article on the same topic, suggesting that isometrics are not necessarily worth the hype (Gravare Silbernagel et al., 2019). That being said, it's not like isometrics are "bad". It's just another type of muscular contraction with some other benefits / weaknesses to it other than concentric or eccentric training. That's why it can be included or not, but is not better than any other muscle action.
Evidence suggests that employing a pain-monitoring model and allowing for adequate adaptation periods during rehabilitation can facilitate ongoing sports participation without negatively impacting recovery.
Adjunct treatment options:
- Platelet-Rich Plasma Injections: Not recommended due to lack of high-level evidence (Scott et al., 2019).
- Transverse Friction Massage: May provide short-term pain relief but lacks long-term efficacy.
- Shockwave Therapy: Mixed results; generally lacking strong evidence.
- Therapeutical Ultrasound: No direct evidence supporting its use in patellar tendinopathy.
- Steroid Injections: Not recommended due to the risk of tendon rupture and lack of long-term benefit.
- Topical GTN/Hyaluronic Acid Injections: Recommended if conservative management fails after 12 weeks (Challoumas et al., 2021).
- Taping: May provide placebo effect and symptom relief.
- Strap Bracing: Recommended for symptom relief during activity (Dar & Mei-Dan, 2019).
- Foot Orthoses: No evidence of direct correlation with patellar tendinopathy.
- NSAIDs: Useful for short-term pain management but not for long-term improvement.
- Cryotherapy: Can be used for pain relief but should be applied after training or competition.
Relying on passive interventions as a substitute for exercise is suboptimal since passive methods have not been demonstrated to normalize tendon matrix, muscle tissue, or address other deficits in the lower extremity.
But if certain treatments help someone feel better and they are also addressing the real key factors of therapy, then they should use them.
Education:
Educating patients on the fact that this is a condition that may take months to cure, that loading is the predominant factor of symptom management and that the sensation of pain during movement / sports is not detrimental and will not lead to a rupture of the tendon is important to reduce fear and increase compliance.
The in season athlete:
For the in season athlete, we want to make sure that we do not simply add one therapeutic exercise on top of another, but that we work on running, jumping and sports-specific technique refinement, which might help desensitising the patellar tendon.
HSR (heavy-slow-resistance) exercise will be our main treatment choice. As results with HRS have been shown to be as good as eccentric exercising, but with greater patient compliance and it aids with tissue normalisation (Muaidi, 2020). And eccentrically biased training would lead to greater muscle soreness, which would be counterproductive for in-season athletes.
The only drawback on HSR training is that it requires a gym, while for eccentric training, to perform the single-leg decline squat, we do not need that.
How to train quads:
When looking anatomically at the quadriceps, we have a four-headed muscle that has a common insertion on the tibial tuberosity, with the main function of knee extension. One head (the rectus femoris) crosses over the hip and aids with hip flexion. This means we can train all four heads with pure knee extension exercises, hit the rectus femoris with hip flexion exercises, and train all the heads (probably with reduced rectus femoris activation, due to its antagonisitc role) with exercises combining knee and hip extension.
Different parts of the rectus femoris muscle will be trained when moving about the hip or the knee due to changes in innervation (different branches of the femoral nerve) across the muscle. Hip flexion will focus on the proximal aspect of the rectus femoris and knee extension on the distal part (Watanabe et al., 2012). This suggests that a variety of exercises including knee extension and hip flexion should be performed to maximise rectus femoris hypertrophy and therefore also quadriceps strength.
In the following we will go through exercises that will load the patellar tendon. Starting with the ones providing the smalles forces onto the tendon, and progressing our way up. This list is adapted form the research findings of Scattone Silva and colleagues (Scattone Silva et al., 2024):
Exercises are split into three tiers. With tier 1 providing low strain, tier 2 for moderate strain and tier 3 for high patellar loading exercises. Needless to say, exercises should increase from tier 1 to tier 3 during rehabilitation.
Tier 1 exercises include: walking, low step up (10 cm), 60º double-leg squat, low step down and high step up (20 cm).
These are the exercises that can be performed for the more sensitive tendons, in the early phases of rehabilitation.
Tier 2 exercises include: high step down, lunge, running, running deceleration, most squat variations (Bulgarian squat, sumo squat...) and jumping exercises.
This study found full depth squats to elicit significantly higher muscle activation and knee strain comparing to the 60º squats. Clinicians should progress the 60º double-leg squat into a 60º single-leg squat and then into a full depth double-leg squat.
As some jumping exercises, such as 1-leg drop landing, 2-leg maximal forward jump and 2 leg drop vertical jump have been put in the moderate loading category, we can probably begin implementing these plyometric exercises sooner than we thought, because the patellar tendon strain is not as high as assumed.
Tier 3 exercises include the single-leg decline squat, run-and-cut, single-leg countermovement hop, single-leg repeated forward hops, and single-leg maximal forward hop.
The single-leg decline squat was the only non-plyometric exercise that generated greater peak tendon loading than running.
All in all: what can we do?
Stretching:
- Test for quadriceps or hamstring flexibility and stretch them out if needed
Mobility:
- Assess for dorsiflexion ROM and if restricted, perform some mobility work.
Load management:
- Reduce overall training load (especially plyometric movements like jumping) at first, then slowly ramp it back up.
Strength training:
- Target specifically the quadriceps muscle to increase patellar tendon loading capacity but also work on hip and ankle strength, to strengthen the whole kinetic chain and thereby reduce the amount of work the knee has got to do.
Technique work:
- For any athlete, utilising the time spent rehabbing should be used to improve exercise / sporting technique which can have a dramatic influence on pain levels.
Lifestyle changes:
- Try fixing your sleep by going to bed and waking up at the same time each day, while getting enough hours of sleep. Also take nutrition into account and make sure you have a balanced diet. If you are in a stressful phase of your life, try implementing some relaxation techniques like yoga nida or meditation into your day to help you calm down.
Adjunct interventions:
- Trying one or two of the adjunct treatments (listed above) for symptom relief can have a positive impact on the patients well-being.
Summary:
Patellar tendinopathy is a condition characterized by pain that worsens with increased load on the knee extensors, particularly during activities that strain the patellar tendon. To effectively rehabilitate patellar tendinopathy, it's crucial to strike a balance between reducing activities that exacerbate pain and gradually increasing tendon strength.
While adjunct treatments like Platelet-Rich Plasma injections, transverse friction massage, and shockwave therapy have mixed or limited evidence, some methods like taping and strap bracing can provide symptom relief. However, passive interventions should not replace the core exercise-based rehabilitation approach.
Education is crucial in managing expectations, emphasizing that recovery is a gradual process requiring several months, and that pain during rehabilitation is not necessarily harmful. For in-season athletes, heavy slow resistance training is recommended to maintain tissue normalization and reduce soreness.
By adhering to these guidelines, patients increase their chances of a successful recovery, enhancing tendon strength and resilience for a pain-free return to their desired level of activity.
Recommendations for this topic:
Literature:
Aicale, R., Oliviero, A., & Maffulli, N. (2020). Management of Achilles and patellar tendinopathy: What we know, what we can do. Journal of Foot and Ankle Research, 13(1), 59. https://doi.org/10.1186/s13047-020-00418-8
Challoumas, D., Pedret, C., Biddle, M., Ng, N. Y. B., Kirwan, P., Cooper, B., Nicholas, P., Wilson, S., Clifford, C., & Millar, N. L. (2021). Management of patellar tendinopathy: A systematic review and network meta-analysis of randomised studies. BMJ Open Sport & Exercise Medicine, 7(4), e001110. https://doi.org/10.1136/bmjsem-2021-001110
Cook, J. L., M Khan, K., S Kiss, Z., Purdam, C. & Griffiths, L. (2001). Reproducibility and clinical utility of tendon palpation to detect patellar tendinopathy in young basketball players. British Journal Of Sports Medicine, 35(1), 65–69. https://doi.org/10.1136/bjsm.35.1.65
Corbi, F., Matas, S., Álvarez-Herms, J., Sitko, S., Baiget, E., Reverter-Masia, J. & López-Laval, I. (2022). Osgood-Schlatter Disease: Appearance, Diagnosis and Treatment: A Narrative Review. Healthcare, 10(6), 1011. https://doi.org/10.3390/healthcare10061011
Dar, G., & Mei-Dan, E. (2019). Immediate effect of infrapatellar strap on pain and jump height in patellar tendinopathy among young athletes. Prosthetics and Orthotics International, 43(1), 21–27. https://doi.org/10.1177/0309364618791619
Dimitrios, S., Pantelis, M., & Kalliopi, S. (2012). Comparing the effects of eccentric training with eccentric training and static stretching exercises in the treatment of patellar tendinopathy. A controlled clinical trial. Clinical Rehabilitation, 26(5), 423–430. https://doi.org/10.1177/0269215511411114
Drakes, S. M. A. (2023). Patellar Tendinopathy: Diagnosis and Management. Current Physical Medicine And Rehabilitation Reports, 11(3), 344–351. https://doi.org/10.1007/s40141-023-00407-5
Gravare Silbernagel, K., Vicenzino, B. T., Rathleff, M. S., & Thorborg, K. (2019). Isometric exercise for acute pain relief: Is it relevant in tendinopathy management? British Journal of Sports Medicine, 53(21), 1330–1331. https://doi.org/10.1136/bjsports-2019-100591
Hannington, M., Docking, S., Cook, J., Edwards, S. & Rio, E. (2020). Self-reported jumpers’ knee is common in elite basketball athletes – But is it all patellar tendinopathy? Physical Therapy in Sport, 43, 58–64. https://doi.org/10.1016/j.ptsp.2020.01.012
Korakakis, V., Kotsifaki, A., Stefanakis, M., Sotiralis, Y., Whiteley, R. & Thorborg, K. (2021). Evaluating lower limb tendinopathy with Victorian Institute of Sport Assessment (VISA) questionnaires: a systematic review shows very-low-quality evidence for their content and structural validity—part I. Knee Surgery, Sports Traumatology, Arthroscopy, 29(9), 2749–2764. https://doi.org/10.1007/s00167-021-06598-5
Lohrer, H. & Nauck, T. (2011). Cross-cultural Adaptation and Validation of the VISA-P Questionnaire for German-Speaking Patients With Patellar Tendinopathy. The Journal Of Orthopaedic And Sports Physical Therapy/Journal Of Orthopaedic And Sports Physical Therapy, 41(3), 180–190. https://doi.org/10.2519/jospt.2011.3354
Maffulli, N., Oliva, F., Loppini, M., Aicale, R., Spiezia, F. & B King, J. (2017). The Royal London Hospital Test for the clinical diagnosis of patellar tendinopathy. M.L.T.J. Muscles, Ligaments And Tendons Journal, 7(2), 315. https://doi.org/10.11138/mltj/2017.7.2.315
Malliaras, P. & Cook, J. (2006). Patellar Tendons with Normal Imaging and Pain: Change in Imaging and Pain Status over a Volleyball Season. Clinical Journal Of Sport Medicine, 16(5), 388–391. https://doi.org/10.1097/01.jsm.0000244603.75869.af
Malliaras, P., Cook, J., Ptasznik, R. & Thomas, S. (2006). Prospective study of change in patellar tendon abnormality on imaging and pain over a volleyball season. British Journal Of Sports Medicine, 40(3), 272–274. https://doi.org/10.1136/bjsm.2005.023846
Malliaras, P., Cook, J., Purdam, C., & Rio, E. (2015). Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. Journal of Orthopaedic & Sports Physical Therapy, 45(11), 887–898. https://doi.org/10.2519/jospt.2015.5987
Muaidi, Q. I. (2020). Rehabilitation of patellar tendinopathy. Journal of Musculoskeletal & Neuronal Interactions, 20(4), 535–540.
Nutarelli, S., Da Lodi, C. M. T., Cook, J. L., Deabate, L. & Filardo, G. (2023). Epidemiology of Patellar Tendinopathy in Athletes and the General Population: A Systematic Review and Meta-analysis. Orthopaedic Journal Of Sports Medicine, 11(6). https://doi.org/10.1177/23259671231173659
Palazón-Bru, A., Rodríguez, M. I. T., Mares-García, E., Hernández-Sánchez, S., Carbonell-Torregrosa, M. Á. & Gil-Guillén, V. F. (2020). The Victorian Institute of Sport Assessment Scale for Patellar Tendinopathy (VISA-P): A Reliability Generalization Meta-analysis. Clinical Journal Of Sport Medicine, 31(5), 455–464. https://doi.org/10.1097/jsm.0000000000000810
Reinking, M. F. (2016). CURRENT CONCEPTS IN THE TREATMENT OF PATELLAR TENDINOPATHY. International Journal of Sports Physical Therapy, 11(6), 854–866.
Scattone Silva, R., Song, K. E., Hullfish, T. J., Sprague, A., Silbernagel, K. G., & Baxter, J. R. (2024). Patellar Tendon Load Progression during Rehabilitation Exercises: Implications for the Treatment of Patellar Tendon Injuries. Medicine and Science in Sports and Exercise, 56(3), 545–552. https://doi.org/10.1249/MSS.0000000000003323
Scott, A., LaPrade, R. F., Harmon, K. G., Filardo, G., Kon, E., Della Villa, S., Bahr, R., Moksnes, H., Torgalsen, T., Lee, J., Dragoo, J. L., & Engebretsen, L. (2019). Platelet-Rich Plasma for Patellar Tendinopathy: A Randomized Controlled Trial of Leukocyte-Rich PRP or Leukocyte-Poor PRP Versus Saline. The American Journal of Sports Medicine, 47(7), 1654–1661. https://doi.org/10.1177/0363546519837954
Silva, R. S., Song, K., Hullfish, T. J., Sprague, A., Silbernagel, K. G. & Baxter, J. R. (2023). Patellar Tendon Load Progression during Rehabilitation Exercises: Implications for the Treatment of Patellar Tendon Injuries. Medicine And Science in Sports And Exercise, 56(3), 545–552. https://doi.org/10.1249/mss.0000000000003323
Sprague, A., Epsley, S. & Silbernagel, K. G. (2019). Distinguishing Quadriceps Tendinopathy and Patellar Tendinopathy: Semantics or Significant? The Journal Of Orthopaedic And Sports Physical Therapy/Journal Of Orthopaedic And Sports Physical Therapy, 49(9), 627–630. https://doi.org/10.2519/jospt.2019.0611
Theodorou, A., Komnos, G. & Hantes, M. (2023). Patellar tendinopathy: an overview of prevalence, risk factors, screening, diagnosis, treatment and prevention. Archives Of Orthopaedic And Trauma Surgery, 143(11), 6695–6705. https://doi.org/10.1007/s00402-023-04998-5
Van Ark, M., Cook, J. L., Docking, S. I., Zwerver, J., Gaida, J. E., Van Den Akker-Scheek, I., & Rio, E. (2016). Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial. Journal of Science and Medicine in Sport, 19(9), 702–706. https://doi.org/10.1016/j.jsams.2015.11.006
Van der Worp, H., Van Ark, M., Roerink, S., Pepping, G., Van den Akker-Scheek, I. & Zwerver, J. (2011). Risk factors for patellar tendinopathy: a systematic review of the literature. British Journal Of Sports Medicine, 45(5), 446–452. https://doi.org/10.1136/bjsm.2011.084079
Watanabe, K., Kouzaki, M., & Moritani, T. (2012). Task-dependent spatial distribution of neural activation pattern in human rectus femoris muscle. Journal of Electromyography and Kinesiology: Official Journal of the International Society of Electrophysiological Kinesiology, 22(2), 251–258. https://doi.org/10.1016/j.jelekin.2011.11.004